Share
When is it safe to practise medicine?
It is with great excitement that I share some very important direction the College received from the CPSA Council on March 1, 2019. With Council’s support, the College will pursue a better understanding of how we can improve patient safety by exploring how concepts like physician impairment, specifically due to fatigue, can impact the delivery of safe health care.
More directly, we need to better understand the impact of physicians practising while impaired.
Now, I understand that the term “impairment” can have some very negative connotations, but I think it’s important to recognize impairment for what it is. There are physicians practising medicine who are not functioning as they should. Their impairment could be the result of fatigue, illness or injury (physical and/or mental), the treatment of those conditions, or last but certainly not least, the use of recreational drugs or alcohol.
The conversation on physician impairment began with dialogue about the legalization of recreational cannabis. This led to much of Council’s discussion on the impact of fatigue on physician performance, but I believe it speaks to the overall concept of physician impairment, which needs to be addressed.
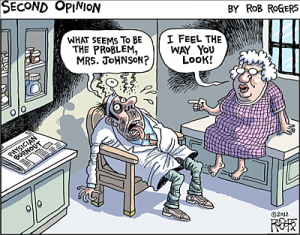
Image source: robrogers.com
Fatigue often occurs as a result of working long or irregular hours, or doing shift or night work, but it also results from family or social responsibilities and lifestyle choices. Fatigue is also unique to different people, but there is evidence to support that fatigue is dangerous. Fatigue changes how we think and make decisions.
I think it’s fair to say it would be inappropriate for a doctor to practise medicine if they were legally intoxicated with blood alcohol concentration (BAC) above 0.08%, yet we ask doctors to perform their duties with the same degree of impairment due to fatigue. There is a great deal of published evidence to support the correlation between fatigue and performance; the vast majority of research has found that when people are without sleep for more than 24 hours, it’s the equivalent of having a BAC of 0.10%. That just can’t continue.
Fundamentally, what we’re talking about is a change in culture for doctors in Alberta and across Canada. It also means that physician leaders will need to take this seriously if we start putting accountability for quality on the agenda for health care in Alberta.
It took decades for the auto, aviation and space industries to recognize the impact of fatigue on safety, but now it is a well and widely-accepted reality of working in those industries. The same culture shift must take place in health care. If we want to take physician burnout seriously and protect patients from potentially dangerous decision making, we need to take physician impairment due to fatigue seriously.
I don’t expect this to change overnight, but the CPSA will be looking into the issue of physician impairment-from a variety of causes-much more seriously over the next year and identifying ways we, as regulators, can help change the culture to better protect patients.
Comments are appreciated,
Scott
























Comments for this post are now closed. If you would like to share your feedback on this topic, please email support@cpsa.ca.